Hypoglycaemia

Hypoglycaemia, or a “hypo” is when your blood glucose levels are too low (below 4mmol/l) due to medication and will usually be associated with symptoms. Anyone’s blood glucose may occasionally drop to just below 4mmols/l when they are hungry – this is safe and will not do you any harm. For patients using insulin or glibenclamide, however, hypoglycaemia is a potentially dangerous side-effect. People using these medications should read on.
What are the warning symptoms?
Hypo warnings vary from person to person. However, you may recognise your own warning signs that indicate your blood glucose level is too low, particularly if you’ve had a hypo before.
Along with shaking, tingling lips or fingers and palpitations you may experience:
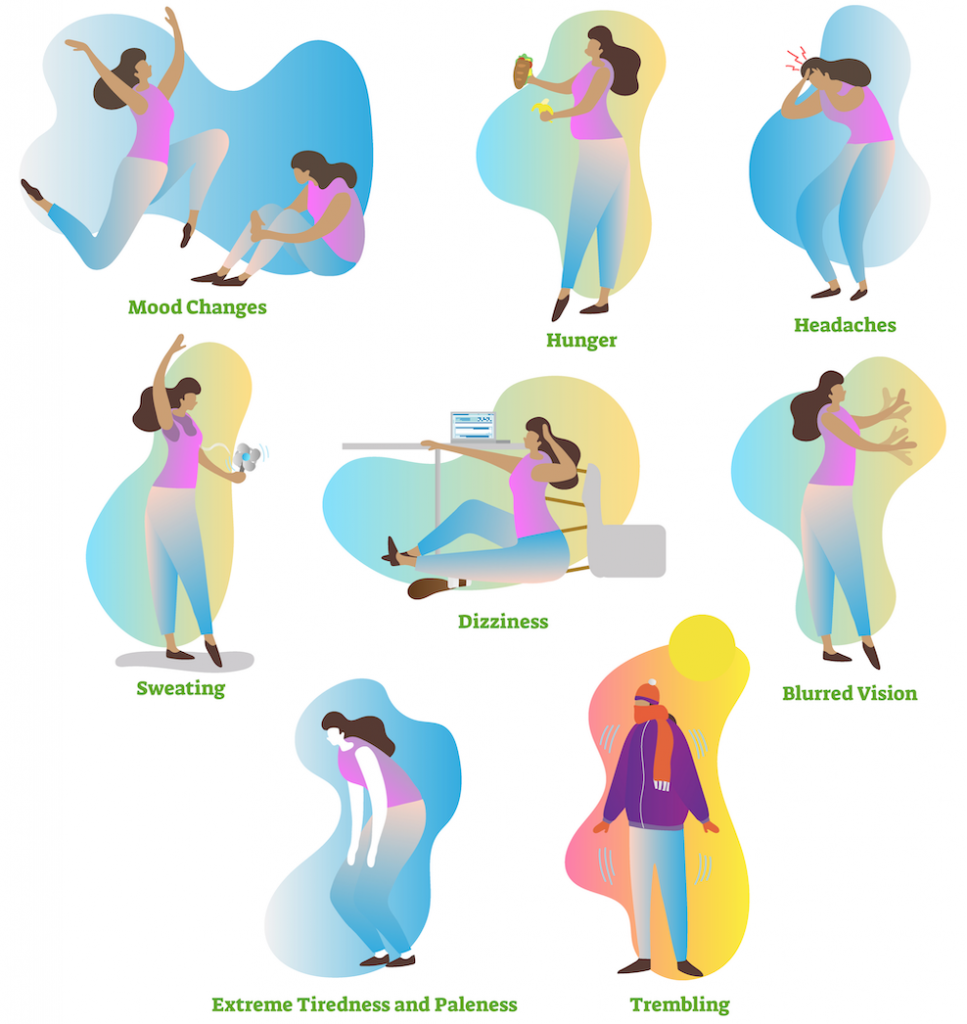
You may not be aware of late warning signs yourself, but other people may notice you becoming pale, moody, aggressive, irrational, confused, unable to concentrate or unable to coordinate your movements.
What sort of things can cause a hypo?
It is important to consider causes of hypoglycaemia in order to prevent them. Causes may include:
- Too little or no carbohydrate at your last meal (for example no bread, pasta, rice, potato, cereal)
- Missed or late meal
- Too much insulin or sulphonylurea tablets(e.g. glibenclamide)
- Exercise – more exercise than usual, for example housework, gardening or sport. Note that a “delayed hypo” can occur several hours after exercise. Always make sure you have a suitable carbohydrate snack after you exercise.
- Alcohol – this may cause you to have a “delayed hypo” overnight or the next day. Always make sure you have a suitable carbohydrate snack or meal after you have alcohol to drink
- A change in injection sites, e.g. changing your injections from an area of lipohypertrophy (“lumpy skin”) to “normal” skin.
- Direct heat or sauna treatment may affect the absorption of insulin and can potentially cause low blood glucose levels if insulin is absorbed more quickly. This can also happen if your insulin is warm – remember that insulin should normally be stored in a refrigerator and kept away from heat and direct sunlight.
- Weight loss (whether intentional or not) or a change in your lifestyle. If you lose weight, then your medication may need to be reduced to prevent hypos.
Occasionally the cause of a hypo may not be obvious. If in doubt, contact your GP, practice nurse or a member of your diabetes team for advice.
How can I treat a hypo?
If you are conscious, and are having a hypo, the best way to treat it is to eat 15-20g of a fast-acting carbohydrate. Examples of fast-acting carbohydrate include sugary non-diet drinks (such as Coca Cola, lemonade or pure fruit juice), glucose tablets, sweets (such as jelly babies) or glucose gel. To prevent your blood glucose dropping low again it is sensible to follow-up this fast-acting carbohydrate with a slower-acting carbohydrate such as a sandwich, biscuit, piece of fruit, or a meal if it is that time of the day.
It is recommended that you check your blood glucose 15-20 minutes after treating your hypo, and treat again if necessary.
For more information on the treatment of hypoglycemia, visit the My Diabetes My Way site.
General advice about hypos
- Always carry some form of rapid-acting carbohydrate – for example dextrose tablets or a non-diet sugary drink.
- Always carry or wear some form of identification specifying you have diabetes and your treatment.
- Tell your friends, relatives, colleagues that you have diabetes and let them know how to recognise a hypo and help if you have one.
- You may have high blood glucose for a few hours after a hypo. This may be caused by the treatment of the hypo and your body’s natural response to hypo.
- Night sweats, morning headache and/or wakening during the night may be symptoms of hypoglycaemia during the night
- You may need to adjust your treatment before exercise to prevent a hypo – ask for advice from your healthcare professional.
- You should not tolerate regular hypos – ask for advice.


Leave a Reply
You must be logged in to post a comment.